COVID-19 outbreaks in hundreds of California nursing homes was ‘an expected disaster’
Six residents of a Woodland nursing home are dead from a coronavirus outbreak that has infected more than 60 patients and employees.
Yolo County announced Tuesday that 31 patients and 33 employees at the Stollwood Convalescent Hospital tested positive for COVID-19.
Under pressure to identify nursing homes with coronavirus outbreaks, the California Department of Public Health last week released a list of 258 facilities with one or more COVID-19 infections among patients or staff. Six are in Sacramento County, three are in San Joaquin County and one apiece is in Placer and Yolo counties.
No facilities in El Dorado County reported cases as of April 17.
The largest nursing home outbreak in the Sacramento region is inside the convalescent hospital, which is part of a Woodland retirement village. Yolo County reported the outbreak on April 13, when one resident had succumbed to the respiratory illness, but did not name the facility until after the state did.
“The loss of life associated with this outbreak is a devastating moment for our community,” Yolo County Public Health Officer Ron Chapman said in a statement Tuesday. “We must acknowledge the suffering of family and friends at this time, who not only lost a loved one, but were unable to be at that individual’s bedside due to the risk of exposure to illness. This fear and uncertainty continues for those that are battling COVID-19 and must remain in isolation. Yet, in the midst of this outbreak, heroic work is occurring to care for and respond to the needs of staff, residents, and families at the facility.”
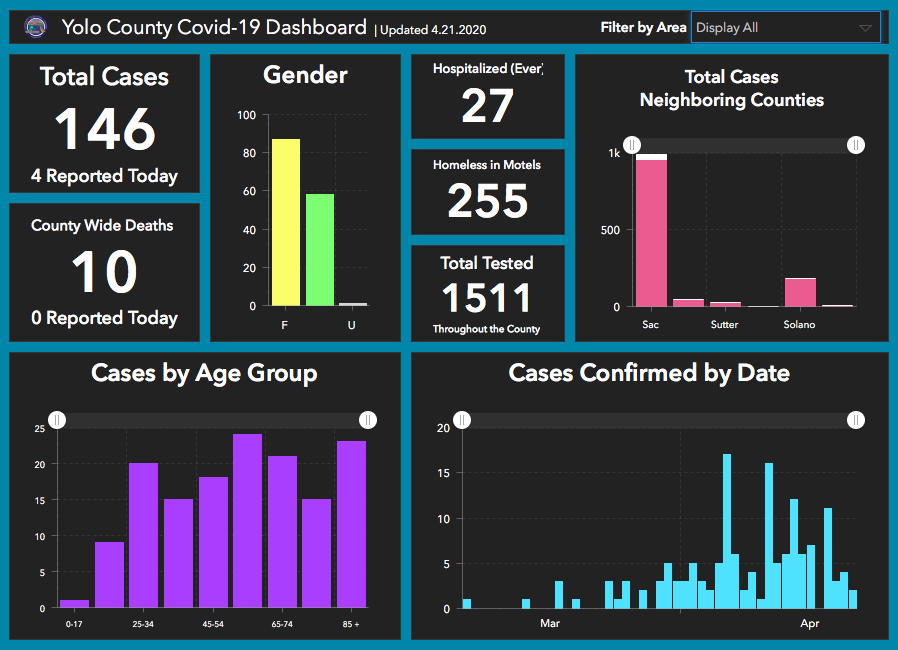
As of April 21, the county reported 146 laboratory-confirmed cases, with 26 hospitalizations and 10 deaths. Fatalities more than doubled in five days and confirmed cases went up 30%.
Half of the county’s coronavirus infections were traced to Woodland, where the Stollwood Convalescent Home is located.
Yolo County spokeswoman Jenny Tan said efforts to contain the outbreak included isolating patients with symptoms, quarantining those with confirmed infections, screening staff before and after their shifts, bringing in food rather than preparing it on site, additional training and setting up PPE donning-and-docking stations in each building, among other strategies.
“A family home line will soon be set up for families of residents to get information about their loved ones,” Tan wrote in an email last week. “Staff at the nursing facility and at Yolo County are working diligently to contain the spread of the virus.”
The ACC Care Center, Casa Coloma Health Care Center, Eskaton Care Center Manzanita, Manorcare Health Services in Citrus Heights, Mid-Town Oaks Post-Acute and Windsor El Camino Care Center—all in Sacramento County—each reported 11 or fewer infections in residents or employees.
But the hardest-hit county is Los Angeles, where 150 facilities have been invaded by the virus.
According to the state’s tracking, a total of 1,740 nursing home patients and 1,290 staff members were infected as of April 17. That equates to roughly 10% of all coronavirus cases in California.
“The data that was recently shared on the persistent, growing and deadly outbreak of COVID-19 in California nursing homes is a clarion call to action for all of us,” April Verrett, president of SEIU Local 2015, which represents more than 385,000 nursing home, home care and assisted living facility workers in California, said in a statement. “This deadly pandemic is targeting our most vulnerable elders. Those charged with caring for them—low wage workers, almost always women—are walking into infection zones without the most basic of protections.
“Raincoats and rags turned into isolation gowns and face masks are not adequate stand-ins for medical grade PPE, or a serious testing regimen.”
As the number of infections climb, industry lobbyists have asked Gov. Gavin Newsom to shield skilled nursing homes from criminal, civil or administrative claims stemming from the outbreaks—an idea that’s drawn vocal opposition from advocates for the elderly and disabled.

Nursing homes seek governor’s protection
During a Monday video conference call to protest “blanket immunity” for nursing homes, members of California Advocates for Nursing Home Reform contended that even before the outbreak, for-profit facilities were short-cutting patient care by not hiring enough staff or paying their workers adequate wages, forcing some employees to work in multiple homes.
Retired geriatrician Teresa Palmer, who has a mother in a nursing home that is accepting COVID-positive patients, said she was terrified by the request and noted that these homes do not have to accept patients for whom they lack the staffing or resources.
CANHR executive director Patricia L. McGinnis and staff attorney Mike Dark said the lobbyists’ proposal would encourage negligence, allowing nursing homes to accept COVID-19 patients whether they had the resources to care for them or not.
“The governor must reject this proposal,” Dark said.
McGinnis chastised the California Department of Public Health, which is responsible for regulating nursing homes, for not doing enough to ensure they’re meeting proper staffing ratios.
“This was an expected disaster waiting to happen,” she said.
The state has taken nearly 2,800 enforcement actions against the industry in the past five years, peaking in 2018 with 625 citations and $6.4 million in penalties. Those figures dipped to 614 citations and $4.8 million in penalties last year, state data shows.
The three single largest outbreaks were at nursing homes the state had taken enforcement actions against in recent years:
- Brier Oak on Sunset in Los Angeles County reported confirmed infections among 80 patients and 62 employees. The state fined the home $45,000 in 2017 for violating three regulations. The investor-owned company reported a net loss of $149,000 in 2015, the most recent year for which profitability data was available.
- Redwood Springs Healthcare Center in Tulare County reported infections among 91 patients and 46 employees. The state leveled $124,000 in fines over the past two years. Also owned by investors, Redwood claimed $840,000 in net income in 2015.
- At Gateway Care & Rehabilitation Center in Alameda County, 69 patients and 33 employees were sickened. Its investors absorbed a $1,000 fine last year and reported a $660,000 profit in 2015.
The state Center for Health Care Quality has fined skilled nursing homes less than $1 million so far this year. While the center has never cited Stollwood for any violations, three Sacramento County facilities with COVID-19 cases have been penalized in recent years. Manorcare and Windsor El Camino were each fined $4,000 last year for two violations apiece, while Mid-Town Oaks was fined $2,000 in 2017.
Jessica Lehman, executive director of Senior and Disability Action in San Francisco, argued that the state should have been doing more to protect its vulnerable nursing home residents and workers long before the pandemic.
“We haven’t been paying attention to people in nursing homes because I think we are subconsciously saying their lives aren’t as valuable,” Lehman said.





Be the first to comment on "Hidden hot zones"